University of Pittsburg and Temple University researchers find acupuncture effective for the alleviation of cancer pain. Acupuncture alleviated additional cancer related concerns including nausea, fatigue, anxiety, and interference with life activities due to pain.  The researchers note that acupuncture reduced pain severity with over 60% of cancer patients “experiencing a clinically meaningful reduction of 30% in pain severity and interference. Acupuncture also resulted in significant improvement in associated symptoms.”
The researchers note that acupuncture reduced pain severity with over 60% of cancer patients “experiencing a clinically meaningful reduction of 30% in pain severity and interference. Acupuncture also resulted in significant improvement in associated symptoms.”
The team of doctors and researchers cited Vickers et al. for the basis of the investigation noting that “acupuncture has been studied extensively showing benefits over placebo for nonmalignant conditions.” Additional research on acupuncture for the treatment of cancer related pain and side effects was cited. Dean-Clower et al. demonstrated that acupuncture reduces cancer related pain in an 8 week study involving 12 acupuncture treatments. The study, involving “women with advanced breast or ovarian carcinoma,” documents a “63% reduction in pain severity and a 75% decrease in pain interference, along with reductions from baseline in anxiety, depression, and fatigue.” Pfister et al. found acupuncture effective for reducing pain and xerostomia while improving functioning for cancer patients. Mehling et al. conducted a study of 138 cancer patients with the acupuncture group experiencing significantly less pain than the control group.
Glick et al. from the University of Pittsburg and Temple University (Pennsylvania) note that Dean-Clower et al. demonstrated greater pain reductions than their study due to three factors. The Dean-Clower et al. patients uniformly had advanced disease, received acupuncture at a larger number of acupoints, and all 12 acupuncture treatments were administered within a more concentrated period of time. Glick et al. note, “The extended duration of the current study, as long as 22 weeks, may have diluted the treatment effect.” They add, “The design of this project was dictated by the primary aim of providing a clinical service.”
Glick et al. note, “This study investigated the effect of acupuncture on cancer-related pain as well as other symptoms, including nausea, fatigue and anxiety. It was found that these symptoms were reduced over a course of treatment involving 9 – 12 sessions of acupuncture. Specifically, pain severity and interference with life activities were significantly reduced with treatment.” A total of 60% of patients had a 30% reduction in pain severity. A total of 36% of patients had 50% reduction in pain intensity. A total of 64% had a 30% reduction in pain interference and 52% had a 50% reduction of pain interference with life activities. Edmonton Symptom Assessment System ratings document a 51% mean reduction of pain, a 49% mean reduction of nausea, a 59% mean reduction of fatigue, and a 44% mean reduction of anxiety.
All patients in the study received standard oncologic and medical care at the Center for Integrative Medicine at UPMC (University of Pittsburg Medical Center) Shadyside or at UPMC Shadyside Hospital (Pittsburg, Pennsylvania). A flexible protocol of 12 acupuncture treatments over a period of 2 - 4 months was made available. The researchers note that the preferred regimen of care was 2 acupuncture treatments per week for 4 weeks followed by an additional 4 weeks of acupuncture at a rate of once per week. Flexibility was allowed to account for hospital admissions, difficulty in scheduling, and personal preferences for treatment times.
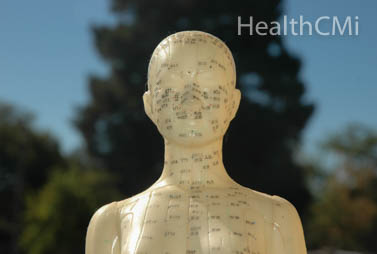
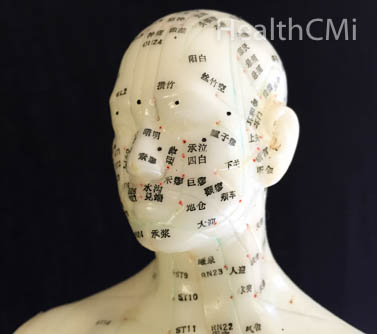
Acupuncture Points
The acupuncture treatment regimen was based on research of Traditional Chinese Medicine (TCM) texts and articles on the treatment of cancer related pain and associated symptoms.
The treatment protocol was designed by 3 licensed acupuncturists and the treating acupuncturist had 7 years of clinical experience. The primary acupuncture points chosen for patients were:
For patients with anxiety, irritability, or agitation the following acupuncture points were added:
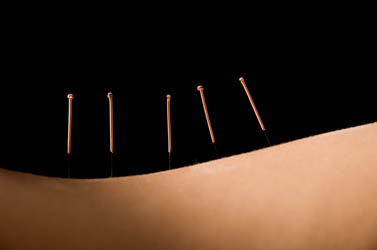
All needles were sterile, disposable, single-use stainless steel needles.
Body point needles were 0.22 x 25 mm and auricular needles were 0.16 x 15 mm.
The researchers note that all body style acupuncture needles were “place to a sufficient depth to elicit De Qi.” The depth typically ranged between 1/2 to 3/4 of an inch.
Manual stimulation was applied with the rotation technique at insertion and later to elicit De Qi for body style acupuncture points not receiving electrical stimulation.
Average needle retention time was 30 minutes and a maximum of 14 acupuncture needles were applied during any acupuncture treatment session.
The flexible treatment protocol allowed for individual customization of acupuncture treatments based on a patient’s needs.
 The researchers note, “This included omitting treatment for any extremity that was involved in lymphatic surgery.” An option to use fewer acupuncture points, shorten the treatment time to 20 minutes, or limit needle stimulation was available for patients that were frail or fatigued. Treatment time was optionally extended to 40 minutes for patients with very severe pain or for slow responders. The researchers add, “at the discretion of the acupuncturist, if other symptoms warranted treatment, modifications to the protocol were allowed to treat additional points.”
The researchers note, “This included omitting treatment for any extremity that was involved in lymphatic surgery.” An option to use fewer acupuncture points, shorten the treatment time to 20 minutes, or limit needle stimulation was available for patients that were frail or fatigued. Treatment time was optionally extended to 40 minutes for patients with very severe pain or for slow responders. The researchers add, “at the discretion of the acupuncturist, if other symptoms warranted treatment, modifications to the protocol were allowed to treat additional points.”
The researchers note that “the vast majority of patients had carcinoma, and the majority had locally invasive or metastatic disease. The majority of patients were actively receiving chemotherapy or other treatment, but several patients were recruited from the Cancer Survivorship Program at the University of Pittsburgh Medical School, Pittsburgh, PA, and were beyond any acute disease-related treatment.” The design of the study bridged the gap between strict acupuncture point protocols required for research and flexibility of acupoint customization needed to reflect a real world acupuncture treatment as it would be applied in a clinic. Given the significant pain reductions and improvements in other conditions, the researchers suggest additional studies investigating the semistructured protocol, pain reduction benefits to cancer patients, and cost savings relevant to health insurance coverage and patient accessibility to acupuncture care.
HealthCMi
At the Healthcare Medicine Institute (HealthCMi), we publish news and research related to acupuncture, herbal medicine, and Traditional Chinese Medicine (TCM). In addition, HealthCMi publishes acupuncture continuing education courses online for licensed acupuncturists to receive NCCAOM PDAs and statewide CEUs. Our online courses include many topics including the treatment of plantar fasciitis, wrist pain, pelvic inflammatory disease, and more.
References:
Glick, Ronald M., Mary Matsumoto, Xiaotian Chen, Yu Cheng, Patricia Smith, Judith L. Balk, Carol M. Greco, and Dana H. Bovbjerg. "Acupuncture for Cancer-Related Pain: An Open Clinical Trial." Medical Acupuncture 27, no. 3 (2015): 188-193.
Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: Individual patient data meta-analysis. Arch In- tern Med. 2012;172(19):1444–1453.
Dean-Clower E, Doherty-Gilman AM, Keshaviah A, et al. Acupuncture as palliative therapy for physical symptoms and quality of life for advanced cancer patients. Integr Cancer Ther. 2010;9(2):158–167.
Pfister DG, Cassileth BR, Deng GE, et al. Acupuncture for pain and dysfunction after neck dissection: Results of a ran- domized controlled trial. J Clin Oncol. 2010;28(15):2565– 2570.
Mehling WE, Jacobs B, Acree M, et al. Symptom manage- ment with massage and acupuncture in postoperative cancer patients: A randomized controlled trial. J Pain Symptom Manage. 2007;33(3):258–266.
 The researchers note that acupuncture reduced pain severity with over 60% of cancer patients “experiencing a clinically meaningful reduction of 30% in pain severity and interference. Acupuncture also resulted in significant improvement in associated symptoms.”
The researchers note that acupuncture reduced pain severity with over 60% of cancer patients “experiencing a clinically meaningful reduction of 30% in pain severity and interference. Acupuncture also resulted in significant improvement in associated symptoms.”The team of doctors and researchers cited Vickers et al. for the basis of the investigation noting that “acupuncture has been studied extensively showing benefits over placebo for nonmalignant conditions.” Additional research on acupuncture for the treatment of cancer related pain and side effects was cited. Dean-Clower et al. demonstrated that acupuncture reduces cancer related pain in an 8 week study involving 12 acupuncture treatments. The study, involving “women with advanced breast or ovarian carcinoma,” documents a “63% reduction in pain severity and a 75% decrease in pain interference, along with reductions from baseline in anxiety, depression, and fatigue.” Pfister et al. found acupuncture effective for reducing pain and xerostomia while improving functioning for cancer patients. Mehling et al. conducted a study of 138 cancer patients with the acupuncture group experiencing significantly less pain than the control group.
Glick et al. from the University of Pittsburg and Temple University (Pennsylvania) note that Dean-Clower et al. demonstrated greater pain reductions than their study due to three factors. The Dean-Clower et al. patients uniformly had advanced disease, received acupuncture at a larger number of acupoints, and all 12 acupuncture treatments were administered within a more concentrated period of time. Glick et al. note, “The extended duration of the current study, as long as 22 weeks, may have diluted the treatment effect.” They add, “The design of this project was dictated by the primary aim of providing a clinical service.”
Glick et al. note, “This study investigated the effect of acupuncture on cancer-related pain as well as other symptoms, including nausea, fatigue and anxiety. It was found that these symptoms were reduced over a course of treatment involving 9 – 12 sessions of acupuncture. Specifically, pain severity and interference with life activities were significantly reduced with treatment.” A total of 60% of patients had a 30% reduction in pain severity. A total of 36% of patients had 50% reduction in pain intensity. A total of 64% had a 30% reduction in pain interference and 52% had a 50% reduction of pain interference with life activities. Edmonton Symptom Assessment System ratings document a 51% mean reduction of pain, a 49% mean reduction of nausea, a 59% mean reduction of fatigue, and a 44% mean reduction of anxiety.
All patients in the study received standard oncologic and medical care at the Center for Integrative Medicine at UPMC (University of Pittsburg Medical Center) Shadyside or at UPMC Shadyside Hospital (Pittsburg, Pennsylvania). A flexible protocol of 12 acupuncture treatments over a period of 2 - 4 months was made available. The researchers note that the preferred regimen of care was 2 acupuncture treatments per week for 4 weeks followed by an additional 4 weeks of acupuncture at a rate of once per week. Flexibility was allowed to account for hospital admissions, difficulty in scheduling, and personal preferences for treatment times.
Acupuncture Points
The acupuncture treatment regimen was based on research of Traditional Chinese Medicine (TCM) texts and articles on the treatment of cancer related pain and associated symptoms.
The treatment protocol was designed by 3 licensed acupuncturists and the treating acupuncturist had 7 years of clinical experience. The primary acupuncture points chosen for patients were:
- PC6
- LI4
- ST36
- KI3
For patients with anxiety, irritability, or agitation the following acupuncture points were added:
- GV20
- Yintang
- Auricular tranquilizer point
- GV20
- Yintang
- HT7
All needles were sterile, disposable, single-use stainless steel needles.
Body point needles were 0.22 x 25 mm and auricular needles were 0.16 x 15 mm.
The researchers note that all body style acupuncture needles were “place to a sufficient depth to elicit De Qi.” The depth typically ranged between 1/2 to 3/4 of an inch.
Manual stimulation was applied with the rotation technique at insertion and later to elicit De Qi for body style acupuncture points not receiving electrical stimulation.
Average needle retention time was 30 minutes and a maximum of 14 acupuncture needles were applied during any acupuncture treatment session.
The flexible treatment protocol allowed for individual customization of acupuncture treatments based on a patient’s needs.
 The researchers note, “This included omitting treatment for any extremity that was involved in lymphatic surgery.” An option to use fewer acupuncture points, shorten the treatment time to 20 minutes, or limit needle stimulation was available for patients that were frail or fatigued. Treatment time was optionally extended to 40 minutes for patients with very severe pain or for slow responders. The researchers add, “at the discretion of the acupuncturist, if other symptoms warranted treatment, modifications to the protocol were allowed to treat additional points.”
The researchers note, “This included omitting treatment for any extremity that was involved in lymphatic surgery.” An option to use fewer acupuncture points, shorten the treatment time to 20 minutes, or limit needle stimulation was available for patients that were frail or fatigued. Treatment time was optionally extended to 40 minutes for patients with very severe pain or for slow responders. The researchers add, “at the discretion of the acupuncturist, if other symptoms warranted treatment, modifications to the protocol were allowed to treat additional points.”The researchers note that “the vast majority of patients had carcinoma, and the majority had locally invasive or metastatic disease. The majority of patients were actively receiving chemotherapy or other treatment, but several patients were recruited from the Cancer Survivorship Program at the University of Pittsburgh Medical School, Pittsburgh, PA, and were beyond any acute disease-related treatment.” The design of the study bridged the gap between strict acupuncture point protocols required for research and flexibility of acupoint customization needed to reflect a real world acupuncture treatment as it would be applied in a clinic. Given the significant pain reductions and improvements in other conditions, the researchers suggest additional studies investigating the semistructured protocol, pain reduction benefits to cancer patients, and cost savings relevant to health insurance coverage and patient accessibility to acupuncture care.
HealthCMi
At the Healthcare Medicine Institute (HealthCMi), we publish news and research related to acupuncture, herbal medicine, and Traditional Chinese Medicine (TCM). In addition, HealthCMi publishes acupuncture continuing education courses online for licensed acupuncturists to receive NCCAOM PDAs and statewide CEUs. Our online courses include many topics including the treatment of plantar fasciitis, wrist pain, pelvic inflammatory disease, and more.
References:
Glick, Ronald M., Mary Matsumoto, Xiaotian Chen, Yu Cheng, Patricia Smith, Judith L. Balk, Carol M. Greco, and Dana H. Bovbjerg. "Acupuncture for Cancer-Related Pain: An Open Clinical Trial." Medical Acupuncture 27, no. 3 (2015): 188-193.
Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: Individual patient data meta-analysis. Arch In- tern Med. 2012;172(19):1444–1453.
Dean-Clower E, Doherty-Gilman AM, Keshaviah A, et al. Acupuncture as palliative therapy for physical symptoms and quality of life for advanced cancer patients. Integr Cancer Ther. 2010;9(2):158–167.
Pfister DG, Cassileth BR, Deng GE, et al. Acupuncture for pain and dysfunction after neck dissection: Results of a ran- domized controlled trial. J Clin Oncol. 2010;28(15):2565– 2570.
Mehling WE, Jacobs B, Acree M, et al. Symptom manage- ment with massage and acupuncture in postoperative cancer patients: A randomized controlled trial. J Pain Symptom Manage. 2007;33(3):258–266.

 Acupuncture successfully reduced both systolic blood pressure (SBP) and diastolic blood pressure (DBP) after 8 weeks of acupuncture treatments.
Acupuncture successfully reduced both systolic blood pressure (SBP) and diastolic blood pressure (DBP) after 8 weeks of acupuncture treatments.
 Acupuncture, as a standalone therapeutic modality, achieved a total effective rate of 85%. The combined herbal and acupuncture therapeutic regimen achieved a total effective rate of 93%.
Acupuncture, as a standalone therapeutic modality, achieved a total effective rate of 85%. The combined herbal and acupuncture therapeutic regimen achieved a total effective rate of 93%.
 The researchers conducted a meta-analysis and concluded that acupuncture significantly improves the overall condition of Parkinson’s disease patients.
The researchers conducted a meta-analysis and concluded that acupuncture significantly improves the overall condition of Parkinson’s disease patients.

 Research published in the International Journal of Traditional Chinese Medicine investigated traditional acupuncture and a new procedure based on acupuncture techniques. Both approaches to patient care were effective in relieving chronic allergic rhinitis.
Research published in the International Journal of Traditional Chinese Medicine investigated traditional acupuncture and a new procedure based on acupuncture techniques. Both approaches to patient care were effective in relieving chronic allergic rhinitis.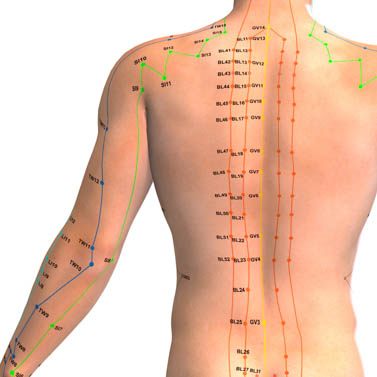
 Additionally, a biochemical analysis reveals that acupuncture regulates expression of MMP-9 (matrix metallopeptidase), an enzyme that breaks down extracellular matrix and is involved in tissue remodeling.
Additionally, a biochemical analysis reveals that acupuncture regulates expression of MMP-9 (matrix metallopeptidase), an enzyme that breaks down extracellular matrix and is involved in tissue remodeling.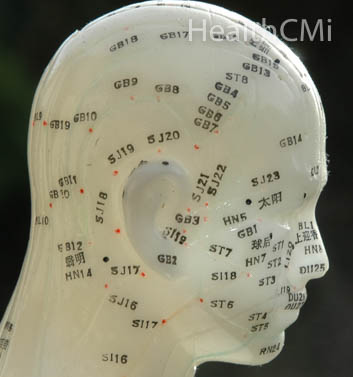 Hence, controlling toxic reactions and cerebral edema is a key factor in the treatment of brain internal bleeding. Yin Nina et al. concluded that pain reduction on patients has a direct impact on the reduction of cerebral edema and controlling MMP-9 expression. Huang Wei has also concluded that cerebral edema can be ameliorated through controlling MMP-9 expression. Prior research demonstrates that acupuncture regulates MMP-9 expression in a homeostatic manner, both in cases of upregulation and downregulation as required by differing medical disorders.
Hence, controlling toxic reactions and cerebral edema is a key factor in the treatment of brain internal bleeding. Yin Nina et al. concluded that pain reduction on patients has a direct impact on the reduction of cerebral edema and controlling MMP-9 expression. Huang Wei has also concluded that cerebral edema can be ameliorated through controlling MMP-9 expression. Prior research demonstrates that acupuncture regulates MMP-9 expression in a homeostatic manner, both in cases of upregulation and downregulation as required by differing medical disorders. The condition may also be referred to as reflex dystrophy syndrome. Researchers conducted a controlled experiment finding acupuncture effective in reducing pain and swelling of the shoulder and hand due to SHS. The total effective rate of acupuncture combined with infrared therapy was 97.10%.
The condition may also be referred to as reflex dystrophy syndrome. Researchers conducted a controlled experiment finding acupuncture effective in reducing pain and swelling of the shoulder and hand due to SHS. The total effective rate of acupuncture combined with infrared therapy was 97.10%. According to Traditional Chinese Medicine (TCM) principles, this acupoint calms the heart and spirit, regulates qi, and suppresses pain. It is located 2 cun above the transverse crease of the wrist between the tendons of the palmaris longus and flexor carpi radialis on the anterior aspect of the forearm. A cun is approximately 1 inch. A cun is a special unit of length measurement used by acupuncturists and is relative to an individual’s physical size.
According to Traditional Chinese Medicine (TCM) principles, this acupoint calms the heart and spirit, regulates qi, and suppresses pain. It is located 2 cun above the transverse crease of the wrist between the tendons of the palmaris longus and flexor carpi radialis on the anterior aspect of the forearm. A cun is approximately 1 inch. A cun is a special unit of length measurement used by acupuncturists and is relative to an individual’s physical size. STC is a type of functional constipation that is present in approximately 15 to 30% of constipated individuals and is characterized by strained bowel movements with lumpy or hard stools. STC involves fewer than three bowel movements per week and is accompanied by a sensation of incomplete evacuation. There may be concomitant abdominal pain, nausea, and low appetite. The incidence of STC increases with age.
STC is a type of functional constipation that is present in approximately 15 to 30% of constipated individuals and is characterized by strained bowel movements with lumpy or hard stools. STC involves fewer than three bowel movements per week and is accompanied by a sensation of incomplete evacuation. There may be concomitant abdominal pain, nausea, and low appetite. The incidence of STC increases with age.
 The results were compared with a traditional acupuncture group and a drug therapy group. The electroacupuncture group had a total effective rate of 96.7% and the traditional acupuncture group achieved an 83.3% total effective rate. The drug therapy group, receiving paroxetine, achieved a 73.3% total effective rate. Based on the findings, the researchers conclude that electroacupuncture at Huatuojiaji and scalp acupuncture points is effective for the treatment of GAD.
The results were compared with a traditional acupuncture group and a drug therapy group. The electroacupuncture group had a total effective rate of 96.7% and the traditional acupuncture group achieved an 83.3% total effective rate. The drug therapy group, receiving paroxetine, achieved a 73.3% total effective rate. Based on the findings, the researchers conclude that electroacupuncture at Huatuojiaji and scalp acupuncture points is effective for the treatment of GAD.
 The research team also investigated the efficacy of electroacupuncture for the treatment of ankle injuries. Warm needle acupuncture combined with herbal compresses achieved a 95% total effective rate and electroacupuncture achieved a 76.7% total effective rate for the treatment of ankle injuries.
The research team also investigated the efficacy of electroacupuncture for the treatment of ankle injuries. Warm needle acupuncture combined with herbal compresses achieved a 95% total effective rate and electroacupuncture achieved a 76.7% total effective rate for the treatment of ankle injuries.
 Indications include infertility, breast milk secretion, amenorrhea, and low sex drive. The researchers discovered that treatment with the drug bromocriptine resulted in a 20% pregnancy rate. When acupuncture was added to the treatment regimen, the fertility rate increased to 43.3%.
Indications include infertility, breast milk secretion, amenorrhea, and low sex drive. The researchers discovered that treatment with the drug bromocriptine resulted in a 20% pregnancy rate. When acupuncture was added to the treatment regimen, the fertility rate increased to 43.3%.


 The SSRI (serotonin reuptake inhibitor) drug sertraline demonstrated a 73.3% total efficacy rate. Conventional acupuncture achieved an 80% total effective rate. Another group received a treatment protocol of Sun Si-Miao’s ghost acupoints combined with sertraline. The combination group achieved a 93.3% total effective rate. The researchers concluded that the combination of acupuncture with drug therapy is safe and effective for the treatment of anxiety and depression due to post-stroke syndrome.
The SSRI (serotonin reuptake inhibitor) drug sertraline demonstrated a 73.3% total efficacy rate. Conventional acupuncture achieved an 80% total effective rate. Another group received a treatment protocol of Sun Si-Miao’s ghost acupoints combined with sertraline. The combination group achieved a 93.3% total effective rate. The researchers concluded that the combination of acupuncture with drug therapy is safe and effective for the treatment of anxiety and depression due to post-stroke syndrome.
 The research confirms that acupuncture exerts an anti-inflammatory action, enhances immunity, and is effective in the prevention of immunological related disease.
The research confirms that acupuncture exerts an anti-inflammatory action, enhances immunity, and is effective in the prevention of immunological related disease.